Interoperability in HealthTech: Experts Insights
Healthcare has long been entangled with inefficiencies, and much like a patient in a maze of endless hospital corridors, it often suffers from a lack of direction—specifically, the lack of interoperability among diverse Electronic Health Record (EHR) systems. As more universal standards are introduced to resolve the issues of competing existing standards, the end result is often just an increase in the number of competing standards.
This cycle highlights the challenge of achieving true interoperability in healthcare, where the goal to streamline and unify data exchange across systems frequently leads to more complexity rather than less. Interoperability, or the ability for health IT systems to talk to each other without needing a translator, is now recognized as a crucial ingredient for the smooth operation of future healthcare systems.
This article draws on some insights from the industry experts at the 2024 HLTH Europe Conference and includes valuable perspectives from our team of specialists in telemedicine app development.
The importance of interoperability in healthcare
Interoperability in healthcare is like having a universal remote for every gadget in your home. Dr. Adam Brown from ABIG Health highlights its necessity, stating, "The ability for different systems to communicate has a profound impact on patients getting the right care," emphasizing that interoperability is as crucial as having a good WiFi signal during a Netflix watch.
Issues with disparate EHR systems
When EHR systems don’t communicate, it's like each department in a hospital using a different dialect of a language. The lack of seamless communication can lead to redundant tests and medical errors—because nothing says 'inefficiency' like having three different radiologists give you three different opinions on the same Xray.
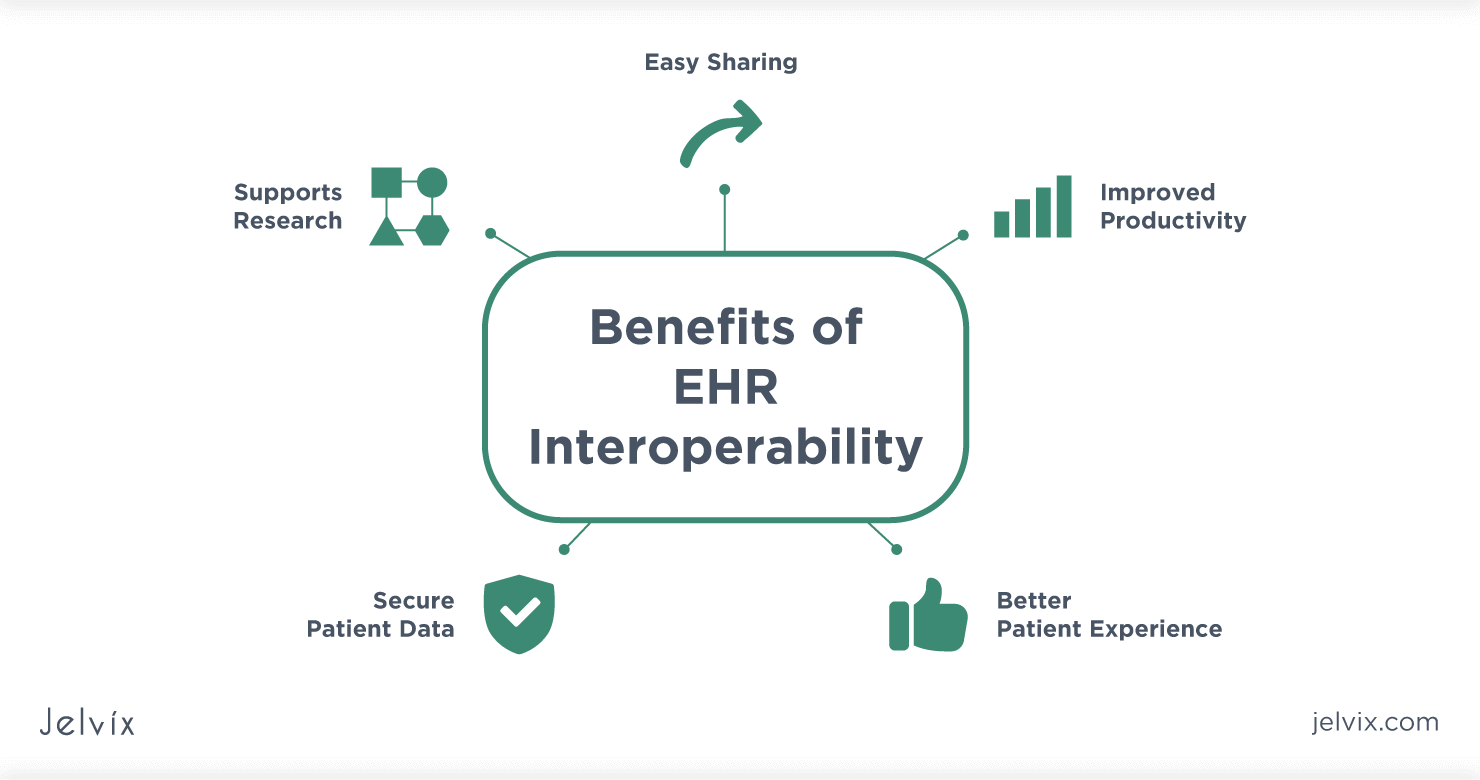
Benefits of seamless data sharing
Seamless data sharing offers benefits that are as clear as a well-organized spreadsheet. Dr. Brown further explaines, "Interoperability benefits patients by improving quality and reducing costs," similar to catching a pricing error in your favor at checkout. For patients, this means less time recounting their medical history and more time discussing f.e. their weekend plans.
General agreement on the necessity of interoperability
The necessity of interoperability is widely acknowledged across the healthcare industry. As stated in insights gathered from healthcare professionals, "the technology breaks down a lot of [administrative barriers] and presents a completely different way of thinking about healthcare,"(Aahuti Rai, Strategic Advisor at Four Points Consulting). The excitement for interoperability is as refreshing as snagging the last seat at a crowded café.
Trends in healthcare interoperability
The industry is moving towards an integrated model where systems not only exist side by side but work together to ensure better patient care, similarly to assembling a team of superheroes each with a unique power. The trend towards greater interoperability is being driven by innovations in health information technology and governmental regulations that encourage or mandate standardized data sharing practices.
Challenges of Implementing Interoperability in HealthTech
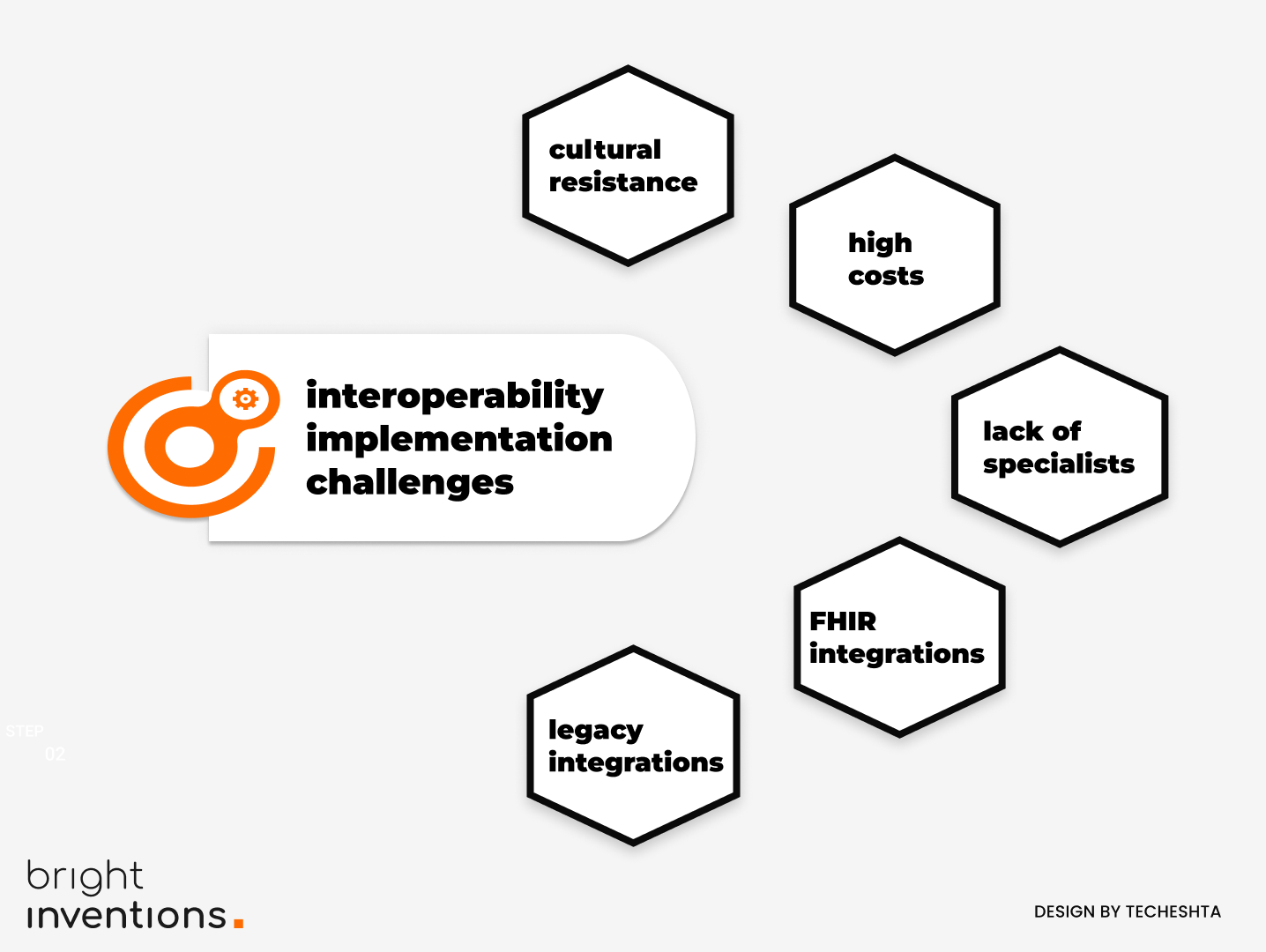
“Implementing interoperability in healthcare is fraught with challenges” - states Maciej Nawrocki, Senior Backend Developer at Bright Inventions - The complexity of modern data standards like Fast Healthcare Interoperability Resources (FHIR) complicates the integration with entrenched legacy systems, often necessitating middleware solutions. These solutions serve as bridges between new and old systems but introduce additional layers that must be managed to maintain data accuracy and consistency.”
Additionally, there is a notable shortage of professionals skilled in FHIR and related standards, making it difficult to find qualified personnel to lead these integration efforts. As the demand for interoperable systems grows, the healthcare industry needs to enhance educational and professional development opportunities in health IT to address these challenges effectively.
HTI-2 sparks optimism with smarter data sharing
The newly proposed HTI-2 rule, as discussed by the Office of the National Coordinator for Health Information Technology, is stirring optimism for further advancing interoperability within healthcare in the US.. This rule is designed to enhance the way health information is shared among patients, providers, payers, and public health entities by setting new standards and introducing robust API capabilities. It aims to tackle the lingering issues of data exchange, cybersecurity, and patient engagement in a more integrated, effective manner. As the healthcare sector pushes towards a more digitally cohesive environment, HTI-2 represents a significant milestone in ensuring that systems not only coexist but also communicate seamlessly to support a truly interconnected healthcare framework. This development could dramatically simplify data handling, making patient care more streamlined and reducing administrative burdens across the board.
Future of Interoperability in Healthcare
In conclusion, interoperability in health tech isn’t just a technical necessity; it’s the cool new trend that’s redefining healthcare. It’s about transforming healthcare from a VHS tape to a seamless streaming service. Dr. Brown sums up the sentiment perfectly: "Interoperability is crucial for efficient, cost-effective, and quality patient care". With technology allowing systems to communicate more freely, the future of healthcare looks not just interconnected but intelligently integrated. This is a journey that requires not only technological advancements but also a cultural shift towards open, shared health data ecosystems.

